The Forum for Democratic Change (FDC) has called on the government to decentralize and integrate mental health services across the country, warning that the current dependency on Butabika Hospital is unstainable.
Speaking to journalists at their party headquarters on Monday, Moses Okwera Mugisha, the FDC Publicity Secretary for Health said that Butabika hospital – formerly designed to accommodate 900 bed capacity is now housing over 1,300 patients, forcing health workers to operate under extreme pressure and leaving many patients without adequate care.
Last week, the media reported that Butabika was sending away some patients because of the overwhelming numbers at the facility amid bedding shortages. Okwera attributed this severe congestion to the government’s underfunding of the sector and failure to strengthen psychiatric services at lower-level health facilities.
“While we commend Dr. Juliet Nakku and her team at Butabika for the incredible work they are doing under pressure, the reality is that mental health has been neglected for too long. Less than one percent of the national health budget is allocated to mental health, yet the cases are increasing every day,” Okwera said.

According to Okwera, the underutilization of psychiatric nurses in local health facilities, many of whom are often redeployed to other departments such as immunization instead of handling mental health patients has left Butabika overwhelmed by cases that could otherwise be managed at the community or district level. He called for decentralization and integration of mental healthcare services to local health facilities and regional referral hospital, schools and families which he says will help to decongest Butabika.
“Decongesting Butabika requires empowering health centers across the country to handle psychiatric clients. Otherwise, one hospital will never be enough for the entire country,” FDC warned.
“We should not keep bringing patients to Butabika,” Okwera added, calling for the established of government rehabilitation centers at Regional Referrals and Mental Health Clinics at Health Centres.
The FDC insists that mental health care should not only be hospital-based but integrated into families, schools and workplaces to reduce stigma and improve early detection of conditions such as depression and schizophrenia.
Additionally, Okwera emphasized the urgency of coping strategies, support networks, and accessible professional care in Uganda to reduce surging cases of suicide which he described as an “extreme” consequence of prolonged depression, and urged citizens to break the silence, and seek professional support against mental disorders.
“If you face a challenge, share it with a friend, colleague, or parent. When it’s beyond what you can handle, visit a health center; counselors, doctors, are there to help.” He reiterated that “suicide is not a solution… the challenge is smaller than the bigger perspective.”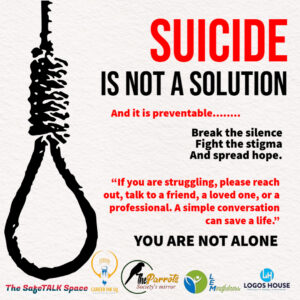
The World Health Organization ranks Uganda among top six African countries with high rates of depressive disorders and having high prevalence of anxiety disorders and PSTD. Around 24% of adults and 22% of children experience mental disorder, with depression and anxiety affecting roughly one in Four. The high rates are linked to factors like conflicts, poverty, drug and substance abuse among others.
Uganda’s 2024 census found that 5.5 million Ugandans, 12% struggle with probable mental mental health conditions such as psychological distress (10%) app. 3.2 million individuals aged 10 and above, depression (8%), bipolar (4%) anxiety disorders (4%), and 1% harbor suicidal tendencies.
Regional data from the Uganda Bureau of Statistics highlight Kampala’s Lubaga Division as a flashpoint, with 6.4% of residents clinically depressed—the highest in the city—closely followed by Kawempe (6.2%) and Nakawa (5.8%). Over the last decade, 272,271 suicidal thoughts or attempts were documented nationwide, with youths aged 10–14 most affected (39,656 cases), then 15–19 (36,615) and 20–24 (34,697).
Additionally, Police data show 218 reported suicides in 2024, up from 165 in 2023 and 235 in 2022, yet experts caution that these figures likely underestimate actual rates due to stigma and criminalization.








































